Grade III pivot shift as an early sign of knee decompensation in chronic ACL‐injured knees with bimeniscal tears
25/08/2021
Magosch A, Jacquet C, Nührenbörger C, Mouton C, Seil R. Grade III pivot shift as an early sign of knee decompensation in chronic ACL-injured knees with bimeniscal tears. Knee Surg Sports Traumatol Arthrosc. 2021 Jul 23. doi: 10.1007/s00167-021-06673-x. Epub ahead of print. PMID: 34302192.
Abstract
Purpose: To analyse possible associations between the preoperative pivot shift (PS) test and both patient and injury characteristics in anterior cruciate ligament (ACL)-injured knees, considering previously neglected meniscal injuries such as ramp and root tears. The hypothesis was that a preoperative grade III PS was associated with the amount of intra-articular soft-tissue damage and chronicity of the injury.
Methods: The cohort involved 376 patients who underwent primary ACL reconstruction (239 males/137 females; median age 26). Patients were examined under anesthesia before surgery, using the PS test. During arthroscopy, intra-articular soft-tissue damage of the injured knee was classified as: (1) partial ACL tear; (2) complete isolated ACL tear; (3) complete ACL tear with one meniscus tear; and (4) complete ACL and bimeniscal tears. Chi-square and Mann-Whitney U tests were used to evaluate whether sex, age, body mass index, sport at injury, mechanism of injury, time from injury and intra-articular damage (structural damage of ACL and menisci) were associated with a grade III PS. Intra-articular damage was further analyzed for two sub-cohorts: acute (time from injury ≤ 6 months) and chronic injuries (> 6 months).
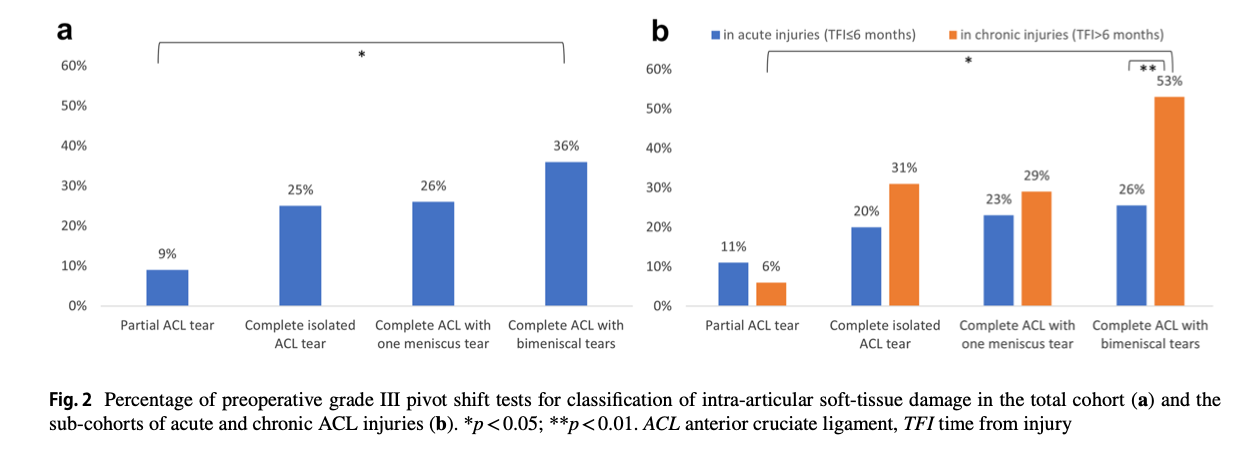
Results: A grade III PS test was observed in 26% of patients. A significant association with PS grading was shown for age, time from injury and intra-articular soft-tissue damage (p < 0.05). Further analyses showed that grade III PS was associated with intra-articular damage in chronic injuries only (p < 0.01). In complete ACL and bimeniscal tears, grade III PS was more frequent in chronic (53%) than in acute knee injuries (26%; p < 0.01). Patients with chronic complete ACL and bimeniscal tears had a grade III PS 3.3 [1.3-8.2] times more often than patients in the acute sub-cohort.
Conclusion: In ACL-injured patients, a preoperative grade III PS was mainly associated with a higher amount of intra-articular soft-tissue damage and chronicity of the injury. Patients with complete chronic ACL injuries and bimeniscal tears were more likely to have a preoperative grade III PS than their acute counterparts. This suggests that grade III PS may be an early sign of knee decompensation of dynamic rotational knee laxity in chronic ACL-injured knees with bimeniscal lesions.
